Optimized layout to improve healthcare
Guideline aims for better accessibility based on changes in demographics

The National Health Commission, together with 12 central and State departments, has issued a guideline for optimizing the allocation of primary healthcare resources to adapt to urbanization and demographic changes.
Aiming to provide better access to safe and effective primary healthcare closer to home, the guideline sets a three-phased goal for developing healthcare providers in the next decade, requiring higher accessibility and significantly improved conditions of the infrastructure by 2027.
By 2030, healthcare providers should be situated in a more balanced and reasonable way, and be able to provide telemedicine and smart health services.
By 2035, the distribution and quality of primary healthcare services should be further improved to support the country's urbanization and rural vitalization efforts, the guideline said.
In China, primary healthcare services are mainly provided by community medical centers based in townships, subdistricts, villages and residential communities.
The layout of services, however, has moved toward taking a new shape in recent years, the National Health Commission said.
"As the (country's) urbanization drive and the readjustment of administrative divisions continue, the number of primary healthcare institutions has been decreasing in rural areas and increasing in urban areas," the commission said in a statement.
As the rural population continues to shrink and get older, and the urban population keeps growing, the layout of medical resources in the country needs to adapt, it said.
The guideline requires every township, a grassroots administrative division often located in rural areas, to operate a health center.
Every village should have a medical clinic, and any excess can be repurposed into medical outlets or other kinds of health institutions, the guideline said, adding that villages with small populations or covering a small area can set up a joint clinic with neighboring villages.
A subdistrict, a grassroots division of a city, should operate one community health service center, the guideline said. Also, if a township changes its administrative status and becomes a subdistrict, its health center should be turned into a community health service center.
Zeng Gang, director of the Institute of Urban Development of East China Normal University, said China's process of urbanization has entailed the readjustment of grassroots administrative divisions, such as merging townships and turning townships into subdistricts.
In this process, the need has emerged to redistribute industries and services, including primary healthcare, Zeng said.
In order to better utilize primary healthcare services, villages that have seen a serious population drain may need to be merged with other villages, or their residents may need to move to places of a higher population density, Zeng said.
Population clustering also helps ensure the sustainability of healthcare providers, he said.
The guideline also requires the improvement of equipment and abilities of clinics in densely populated villages.
Health service stations should also be set up in large and densely populated urban neighborhoods that are located beyond the reach of a community health service center, it said, adding that the scale of such stations should be expanded appropriately.
The guideline requires relevant authorities of provinces, autonomous regions and municipalities to fully consider differences among regions when optimizing the number and location of primary healthcare institutions.
They should avoid closing institutions indiscriminately, leading to reduced service accessibility, while preventing underutilization of medical resources, it said, urging them to prioritize efforts to improve institutions in less-developed areas.
Zeng, the researcher, said new and holistic approaches are needed to ensure efficient and quality allocation of medical resources and other infrastructure in rural areas.
He suggested local authorities prioritize the development of rural areas in their spatial planning, and come up with a comprehensive infrastructure plan that coordinates efforts among different government departments.
China has taken a series of measures over the years to funnel high-quality resources to grassroots health institutions and raise their service quality.
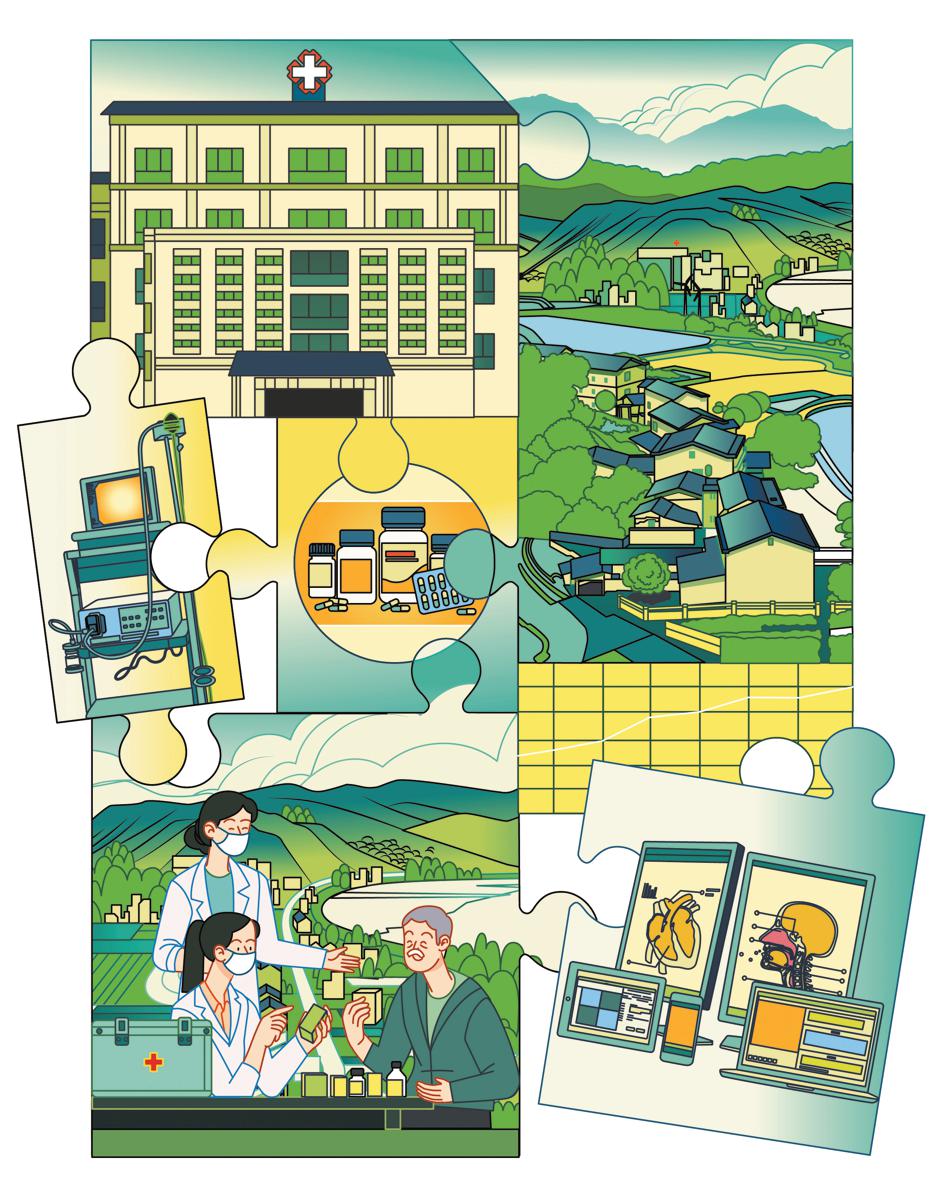
At the end of 2023, the country started promoting the construction of "tightly knit medical consortia" in all of its counties, aiming to establish them in at least 90 percent of all counties by the end of this year.
Such consortia are made up of county-level hospitals, township-level health centers and village clinics. All these entities are expected to work closely, share their resources and be managed as a unit.
County-level hospitals should play a leading role in supporting grassroots health institutions, according to Lei Haichao, head of the National Health Commission, who said in March that the commission will advance its work this year to build the consortia.
The guideline follows on from the initiative, urging medical institutions in counties, townships and villages to strengthen integration, and calling for the acceleration of the redeployment of healthcare professionals and other resources to grassroots health institutions.
Liu Yuanli, a professor at Peking Union Medical College, said a tightly knit medical consortium aims to turn different health institutions that sometimes compete with each other into "one family", and boost the members' willingness to assist each other.
It will also help set up a tiered system of diagnosis and treatment where patients are first treated at the grassroots level, Liu said.
Without the tiered system, people tend to avoid grassroots health service providers nearby and choose to visit large hospitals directly, increasing their own costs and depriving the critically ill of essential resources, he said.
The guideline also calls for establishing "resource sharing centers" for different health institutions in a county to share resources of laboratory testing, imaging, electrocardiogram diagnosis, pathological diagnosis and sterilization, thus enabling primary healthcare institutions to conduct tests while higher-level hospitals to make diagnoses based on the test results.
The resource sharing centers can help prevent excessive investment into functional and supportive departments, Liu said.
The researcher in health policy and management called for further building up county-level hospitals, saying the ability of these hospitals can determine that of a county's grassroots health institutions.
"Many county-level hospitals are facing not only heavier workloads, but also increased challenges, including a loss of experts and patients to hospitals at a higher level," he said.
Artificial intelligence technologies can play a part in improving the performance of grassroots health institutions, he said, adding that AI-driven large models "are imposing rapid and far-reaching influence on the quality and efficiency of healthcare service".
wangqingyun@chinadaily.com.cn
- Police punish shopper after AI video used in fake crab claim
- Historians identify Chinese pilot saved by John Rabe in Nanjing
- Rainforest-themed activities launched in Hainan
- Hebei advances intelligent construction and prefabricated housing
- Seventh Hainan Island International Film Festival opens in Sanya
- Former chairman of Guangxi government expelled from CPC, public office